Introduction
- Glaucoma (aka “Kala Motia” in Hindi) is also known as “Silent thief of Sight”, as patients suffering from advanced glaucoma gradually develop irreversible blindness and tunnel-like vision. Patients with advanced glaucoma are not even able to perform their daily routine tasks effectively.
- Glaucoma is very characteristically known by the optic nerve changes and progressive damage to the optic nerve. The changes in the optic nerve results in the characteristic disc appearance and corresponding changes in the visual field.
- The cause for maximum cases is unknown and therefore, primary glaucoma is either idiopathic or has some genetic cases which are yet not precisely known.
- Raised Intraocular Pressure (IOP) is not a part of the definition of glaucoma, as it is just a risk factor.
Broad Classification
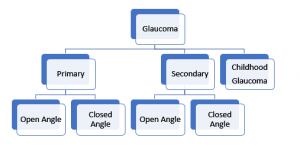
- Classification helps to plan a treatment strategy
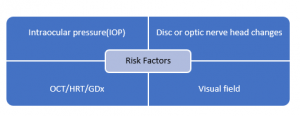
Key players of diagnosis
For the precise diagnosis, there are five things to keep in mind:
Elaborating the above-mentioned key players in detail:
- Intraocular pressure
Normal IOP:
- According to the studies, normal IOP has a very wide range but for practical purposes, Mean IOP (GAT): 15±3 mmHg (Range 12-18) is considered.
- The “magic number of 21” is a figure of the past, an obsolete concept.
- In a graphical representation, Normal distribution with a slight skew towards higher values is seen.
- Remember many factors, in addition to glaucoma, influence IOP and can be divided into 2 categories (i) those that exert a long-term influence (e.g., genetics, age, gender, refractive error, and race), and (ii) those that cause short-term fluctuations in the pressure (e.g., time of day, body position, exertion, lid, and eye movement, various ocular and systemic conditions, general anesthesia, and some food and drugs).
Diurnal variation of IOP:
- IOP doesn’t remain the same throughout the day.
- IOP value is generally higher in the morning than in the afternoon; normal fluctuation is about 2-5 mm Hg in a day.
- If the fluctuation is not in the normal range within a day, then this IOP damages the optic nerve over a prolonged period.
Applanation Tonometry:
- Clinically, Goldmann Applanation Tonometer (GAT), a gold standard tonometer is used to measure the IOP. This is one of the most reliable ways of measuring the IOP.
GAT is mounted on a slit lamp and the patient sits on the other side. In the biprism of the applanation tonometer, the doctor can see two green mires under a cobalt blue filter and the endpoint of the pressure is reached when the inner margins of these superior and inferior hemispheres touch each other.
NOTE: Never start treating the patient based on one reading of IOP. Make sure to take 2-3 different readings at different periods on different days to ensure the most reliable reading of IOP.
IOP Paradox:
“Everything within 12-18 mm Hg range is not normal and everything beyond 18 mm Hg is not abnormal”.
There are two paradoxical conditions:
- Paradox 1: When there is GON, i.e., Glaucomatous optic nerve damage but the IOP < 21 mmHg, there is damage to the nerve and visual fields. This entity is called Normal/ Low Tension Glaucoma (NTG/LTG).
- Paradox 2: When the IOP value is > 21 mmHg and there is no optic nerve damage and the visual fields are perfectly fine, this entity is known as Ocular Hypertension (OHT; Normal variant).
NOTE:
- Remember, Refrain from using the word “Normal” in the clinical case scenarios because a range that is normal for one may not be normal for the other.
- If baseline IOP is > 30 mmHg, it is reconfirmed once and the patient should be started on therapy without the need for performing a diurnal IOP recording.
Central Corneal Thickness (CCT):
- It is measured by an instrument named Pachymeter.
- Normal corneal thickness is around 520-550 microns.
- It is an independent predictor of Glaucoma.
- Goldmann applanation tonometer calibrated for CCT of 520 mm: a thinner CCT underestimates true IOP, and thicker CCT overestimates.
- A very thin or very thick cornea can impact the decision-making process regarding the need to treat, or the aggressiveness of the therapy.
-
Optic Disc/ Optic Nerve Head: Normal Vs. Glaucoma
In the optic disc, the central part which is paler than the peripheral part is called the cup, and the reddish-orange part over the cup is called the neuro-retinal rim (NRR)and the entire neural tissue lies here.
There are a few things we need to consider, for the cup is to disc ratio measurement mentioned below:
- We can consider Optic disc as a ‘Donut’. The central part is empty, i.e., non-neural tissue but the peripheral part has neural tissue (NRR), and we should focus on the health of NRR.
- Cup: Disc Ratio: The central part is the cup and the blood vessel are coming and bending out on the neural rim. It is referred to as Cup Diameter/ Disc Diameter.
- Colour Cup: We must not interpret cupping by just looking at the color of the cup.
- Contour Cup: The important point to consider is the bend of the blood vessels coming out of the blood. It tells the exact margin of the cup.
- Correlate with the disc size: Usually, large discs have large cups and this cupping is physiological. However, a small disc with even a small cup must be examined with caution as it is more prone to develop glaucoma because the nerve fibres are tightly packed. Glaucomatous eyes with small discs may have pseudonormal cups.
- High interindividual variability: There is an immense amount of variability in individuals of the same race and in different races.
- ISNT Rule:
- It is the health of the neural rim that accounts for the health of the optic nerve.
- As a rule, the inferior neural rim of the optic disc is the thickest followed by the superior rim followed by the nasal rim, and the temporal rim is the thinnest. This is called the ISNT Rule.
- Nearly 80% of healthy optic nerves follow the ISNT rule. 20% of normal individuals can have different thicknesses of the rims but with all the other tests, we can rule out glaucoma in those individuals.
- In advanced cases of glaucomatous optic neuropathy, there occurs concentric NRR loss.
Glaucomatous Optic Neuropathy (GON):
- Glaucoma is a disease that begins with asymmetry. Initially, the cupping in one eye is different from the other eye. When the asymmetry of the cup: disc ratio between the two eyes is more than 0.2, a person is labelled as Glaucoma Suspect.
Characteristics features of GON include:
- Generalized or focalized increase in the optic cup size and the cup: disc ratio
- Vertical enlargement of the optic cup (especially at the superior and inferior poles)
- Asymmetric cupping (0.2 cup-disc ratio difference) between the two eyes
- Narrowing or notching of the neural rim
- Splinter/ Drance hemorrhages
- Changes in vessel configuration and caliber
- Increased visibility of the lamina cribrosa pores
Accurate documentation with an optic disc drawing at baseline is important and can be supplemented with stereo-optic disc photography. Changes in disc findings are more sensitive indicators of the presence and progression of the disease
- Gonioscopy
- To classify the anterior angle chambers into Open Angle Glaucoma and Closed Angle Glaucoma, a lens called a Gonioscope to view the angles.
- Why can’t we see the anterior chamber angle with the slit lamp or direct observation?
There is a small protrusion of the scleral tissue which projects anteriorly to the angle just like the watch glass fitted into the rim of a wristwatch. Similarly, because of the projection of scleral tissue, the cornea is fitted like a watch glass. There is a total internal reflection at the cornea-air interface and the light rays do not get out to reach our eyes. So, the curvature of the cornea creates internal reflection and therefore we need an additional lens called a Goniolens.
- What does a Goniolens do?
Gonio lens permits the visualization of the angle by eliminating the cornea as a refracting surface by placing a concave surface against the cornea.
So, these different glasses allow visualization of the angles using obliquely inclined mirrors.
-
- What if the angles are closed?
- Once angle closure is diagnosed, categorize the stage of angle closure
- Find out the whether the angle closure is appositional or synechial. If the goniolens. is pressed in the centre of the cornea, the aqueous from the centre is displaced towards the angle and open it up artificially. This means that the angle closure is appositional. But if there were adhesions between the iris and the cornea or the lens, there are synechia, then whatever amount of displacement of aqueous is there, it will not open the angles and this is called Synechial angle closure.
- When to do gonioscopy?
All Glaucoma patients need to undergo:
-
-
- Initial examination
- Repeat every 1-2 years as the human body is dynamic and with age, health conditions keep on changing
-
- What is seen through the Goniolens?
- Schwalbe’s line (SL)
- Trabecular meshwork (TM)
- Scleral spur (SS)
- Ciliary body band (CBB)
In Secondary Glaucoma,
- Pigmentary Glaucoma: Mascara line is seen which has a lot of pigments.
- Pseudoexfoliation Glaucoma: Sampolesi’s Line
- Angle recession: Seen in the case of trauma
- NVG: Abnormal blood vessels as seen in the Neovascular Glaucoma.
- Visual field
- Visual field testing is known as Perimetry.
- Up to 37% of optic nerve fibers need to be lost before a VFD is found on automated perimetry, usually progressing from mid-peripheral or paracentral VFD in the earlier stages, to loss of central fixation points and temporal visual field loss in advanced
- Standard automated full-threshold static perimetry is preferred; use the same test strategy for comparison.
- Glaucoma visual field defect respects the horizontal meridian. Defects respecting vertical meridian, are likely due to neurophthalmic problems.
- Reliable tests are crucial and influenced by learning, patient comprehension and cooperation, artifacts, and other ocular pathology.
- Characteristic traits of glaucomatous visual field defects:
- Asymmetrical along the horizontal midline
- Located in the mid periphery(5-25° of fixation)
- Reproducible
- Not attributable to any other pathology
- Localized
- Correlating with the appearance of optic disc
- Whenever there is thinning of the inferior neuro-retinal rim, there will be superior optic nerve defect and vice versa.
- After analyzing the structural changes, match them with the corresponding functional defects.
- Retinal nerve fibre layer (RNFL) analysis: RNFL thinning detected with optical coherence tomography (OCT) is useful to diagnose early glaucoma. Use in conjunction with the other parameters.
- Risk Factors
- Elevated IOP
- Myopia
- Optic nerve changes
- Family history of glaucoma
- Increasing age
- Race
- Diabetes mellitus
- Cardiovascular disease
Treatment:
The main goals of treatment are:
- To preserve visual function with stable optic nerve and visual field status in the patient’s lifetime, by controlling IOP within the target range and addressing other risk factors, and
- To maintain quality of life.
IOP lowering by medication, laser, or surgery is the mainstay of treatment to prevent glaucoma development and retard progression.
(Detailed discussion in a subsequent blog)
Putting it all together!!
- Does this patient have glaucoma?
- If not, how high is the risk of developing glaucoma?
- What other tests need to be done?
- When do you see this patient back?
- When/How do you start treatment?
- What is the prognosis for this patient?
‘Basic Toolkit for Glaucoma’ by Dr. Parul Ichhpujani
To get conceptual clarity in Ophthalmology online, subscribe to CBME & NEET-oriented Ophthalmology for UnderGrads course.
Dr. Parul Ichhpujani
MS, MBA
Professor at Glaucoma Services
Department of Ophthalmology, Govt. Medical College and Hospital, Chandigarh, India

